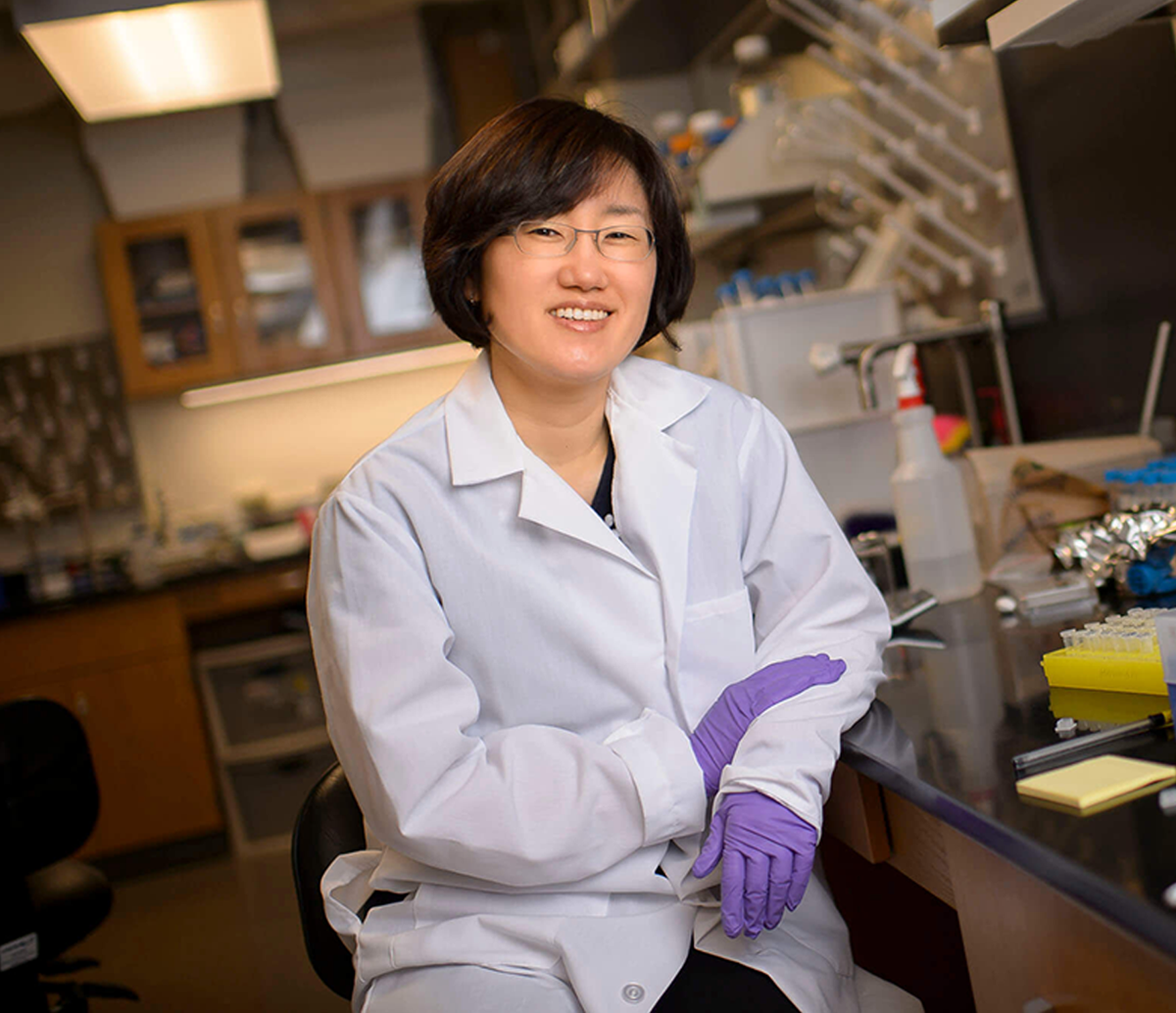
Yoon Yeo and team create biocompatible nanoparticles to enhance systemic delivery of cancer immunotherapy
Immunotherapy is a promising approach to fighting cancer. A team led by Yoon Yeo of the Purdue Institute for Cancer Research, Purdue University College of Pharmacy, and Purdue Institute for Drug Discovery, is developing nanoparticles to make it even better. These innovative researchers are developing and validating patent-pending nanoparticles modified with adenosine triphosphate, or ATP, to enhance immunotherapy effects against malignant tumors.
Research
Give Now
Events
Tyler Trent Pediatric Cancer Research Center
In creating the Tyler Trent Pediatric Cancer Research Center, the Purdue Institute for Cancer Research (PICR) brings together deep strengths in multiple research fields to fight pediatric cancers and to beat osteosarcoma, the rare bone cancer that took the life of beloved Purdue alumnus Tyler Trent.
Tyler’s parents, Tony and Kelly Trent, lead the way with their gift of $100,000 to continue the fight against cancer that Tyler began. To join in the fight, you can donate here to the center’s life-sustaining research.





Twitter feeds
@19830d